Community Health Profile
Sunshine Coast
Community Health Profile
Sunshine Coast
This report provides an overview of health and wellness on the Sunshine Coast that will give residents, community agencies and local governments a better understanding of the factors influencing health in their community. Our hope is that this information will help spark community level dialogue on actions to create health promoting environments and reduce health inequities.

Highlights
- Significantly higher self-reported general health and mental health compared to health authority and regional average.
- Relatively higher prevalence of obesity and chronic diseases such as high blood pressure and arthritis and cancer.
- Relatively car dependent region with potential opportunities for increasing active forms of transportation as most journeys for regular commute are of short duration.
- Overall exceptional elements of community resiliency with higher than average personal emergency preparedness, strong sense of community belonging and low food insecurity.
- These community level data will contribute to the partnership work with regional district.
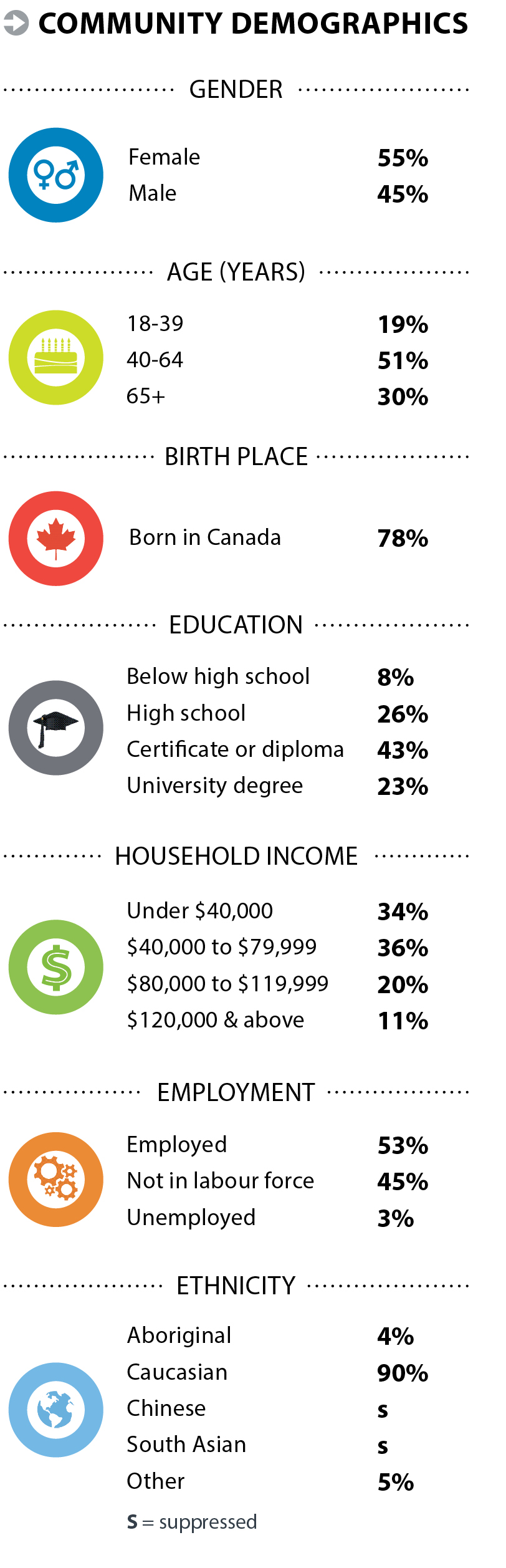
Community Demographics
Healthy Behaviours
Healthy behaviours contribute to maintaining physical and mental health, and reducing the risk of chronic conditions such as heart disease, diabetes and stroke. Recommended lifestyle behaviours include (but are not limited to) consumption of 5 or more servings of fruits and vegetables per day, limiting harmful alcohol consumption, avoiding smoking, exercising moderately to vigorously for 150 or more minutes per week, and reducing screen time and other sedentary activities.
Healthy behaviours are shaped by individual choices, social and economic conditions and neighbourhood design. Community programs and policies can encourage and enable healthy behaviours and reduce the burden of chronic conditions in our communities.
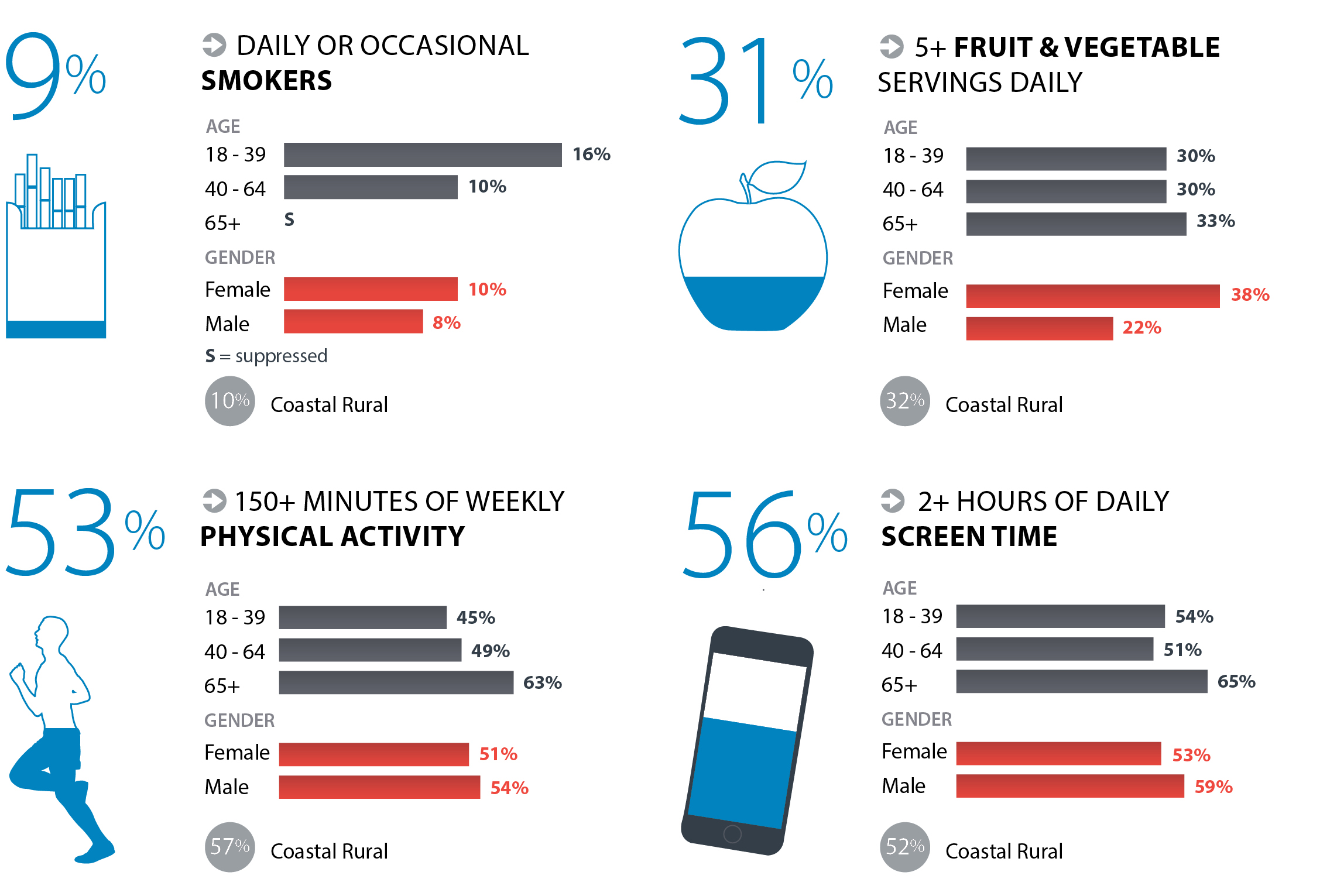
Across Coastal Rural
- Healthy behaviours were higher among people with annual household income greater than $120,000. They were less likely to smoke, more likely to consume 5+ daily servings of fruits and vegetables and less likely to report 2+ hours daily screen time compared to those with household income under $40,000.
- Healthy behaviours differed by ethnic groups. Compared to the Coastal Rural average, smoking was 2 times higher and consumption of 5+ daily fruit and vegetable servings was 50% lower among Aboriginal people.
- Healthy behaviours were higher among university graduates compared to those with less than high school education. They were 85% less likely to smoke, more than 2.5 times more likely to consume 5+ daily servings of fruits and vegetables, more likely to get 150+ minutes of weekly physical activity and almost 50% less likely to report 2+ hours of daily screen time.
- Canadian born were more likely to eat 5+ daily servings of fruits and vegetables, but 4 times more likely to be smokers compared to immigrants.
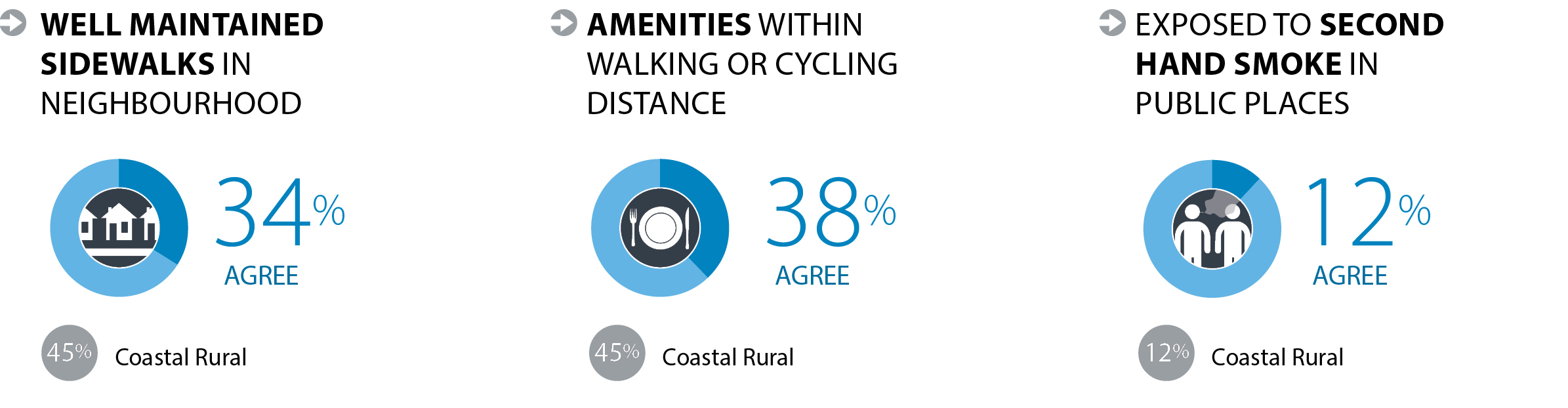
Built Environment
The physical environment in which we live, work and play impacts our health. Physical components of a built environment include neighbourhood design, transportation networks, natural environment, healthy food systems and housing. Community design influences community connectedness, mental and physical health, and chronic disease outcomes by promoting healthy behaviours such as walking or cycling. Healthy built environments are a shared responsibility and require the combined efforts of community agencies, health and social services and various levels of government.
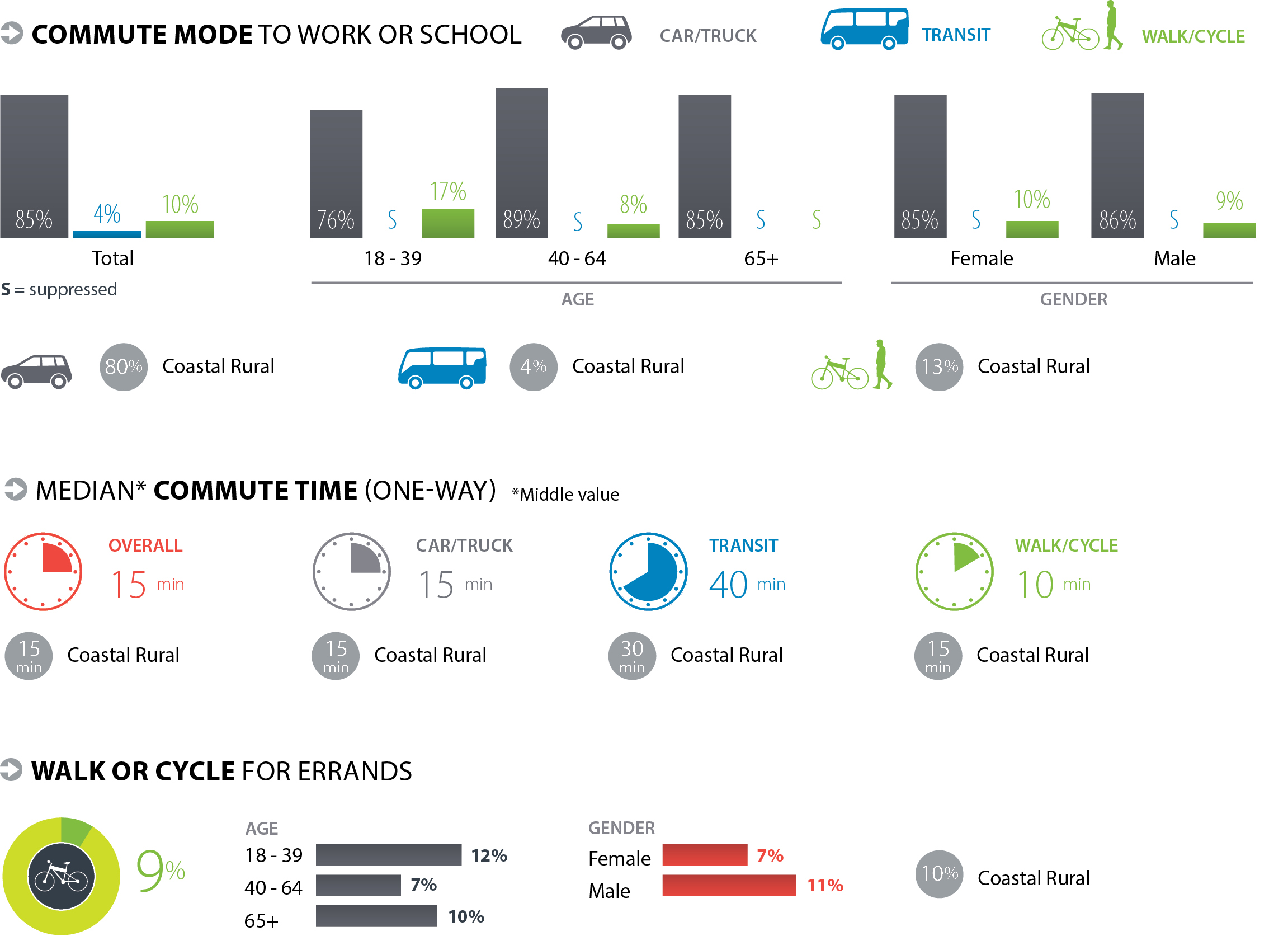
Across Coastal Rural
- Commuting by car was almost 40% higher among those with annual household income greater than $120,000 compared to those with income less than $40,000. Commuting by walking or cycling was 50% lower among those with income greater than $80,000 compared to those with income less than $40,000.
- Exposure to second hand smoke in public places was lower among university graduates compared to those with less than high school education.
- Compared to Canadian born, recent immigrants were 40% less likely to commute by car and more likely to commute by transit.
Community Resiliency
Support from families, friends and communities is associated with better health as it helps people deal with challenges and overcome problems. Supportive communities provide environments in which people are able to make decisions to improve their health and engage in healthy behaviours.
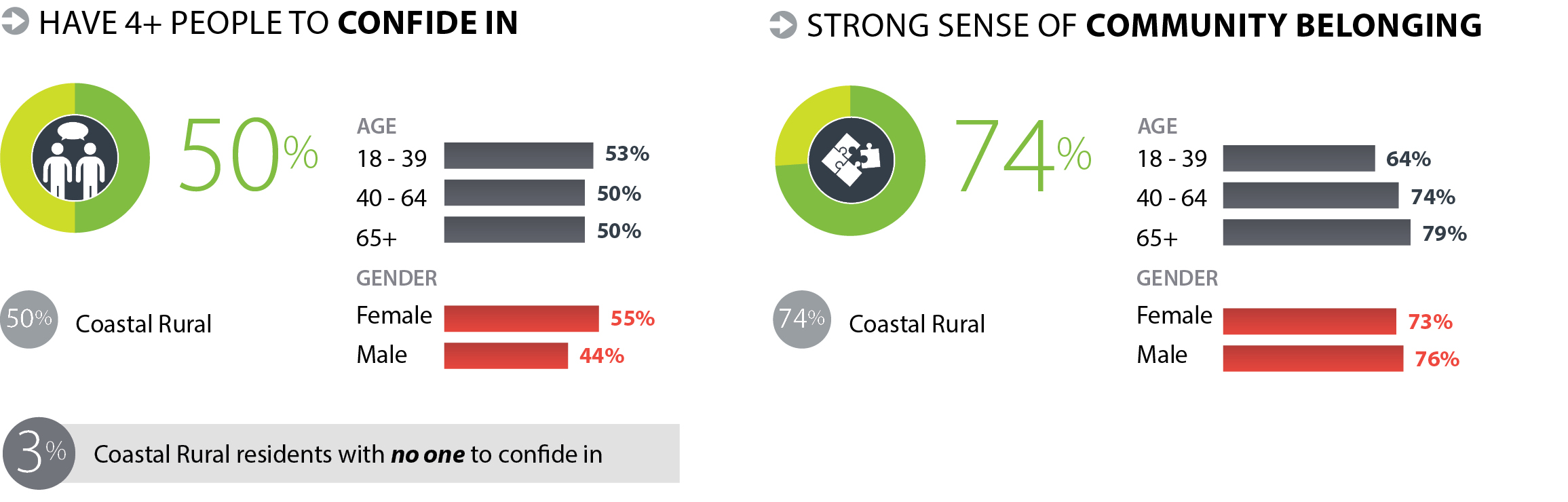
Across Coastal Rural
- Recent immigrants were less likely to report having 4+ people to confide in compared to Canadian born.
- Those with annual household income of $120,000+ were more likely to report having 4+ people to confide in.
- University graduates were more likely to report having 4+ people to confide in.
- Compared to the Coastal Rural average of all ethnicities, Aboriginal people were 35% less likely to report having 4+ people to confide in.
Family Doctor
Having a family doctor plays an important role in maintaining health and preventing chronic illness. Regular contact with a health care provider ensures that recommended preventive services, like screening for early stages of disease, is timely and that chronic conditions are well-managed to prevent complications. Having a regular care provider also helps to maintain continuity of care.
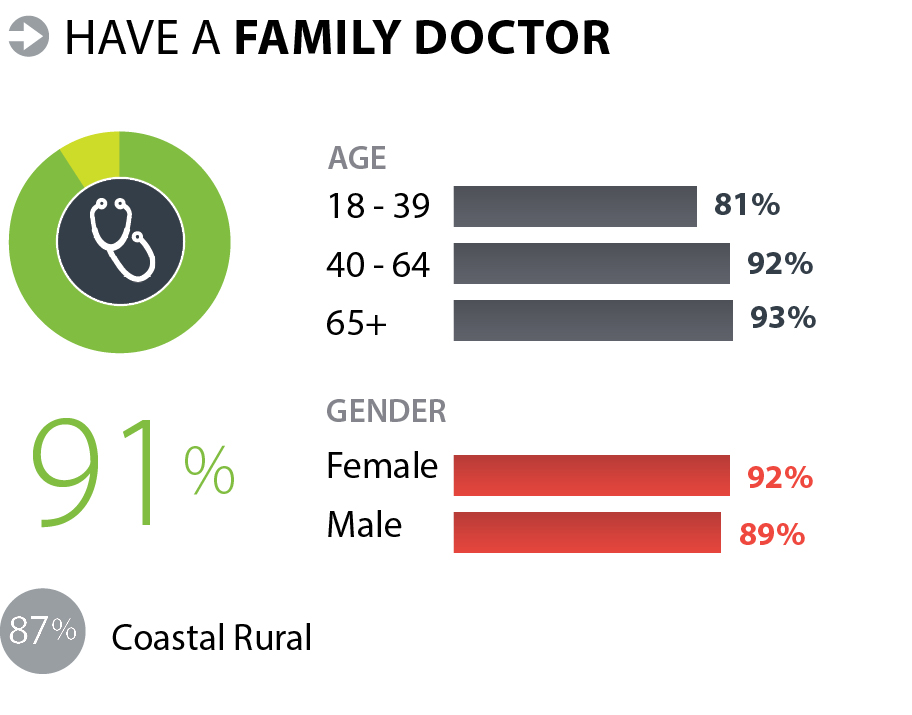
Across Coastal Rural
- Compared to the Coastal Rural average, having a family doctor was 40% lower among recent immigrants.
- People with annual household income of $120,000+ were 15% more likely to have a family doctor compared to those with household income under $40,000.
- Having a family doctor did not differ by education level.
Health Status
Our physical and mental health is influenced by lifestyle behaviours, access to health services, the built environment, and our social and economic situation. Self-rated health is considered to be a good measure of the general health status of a population.
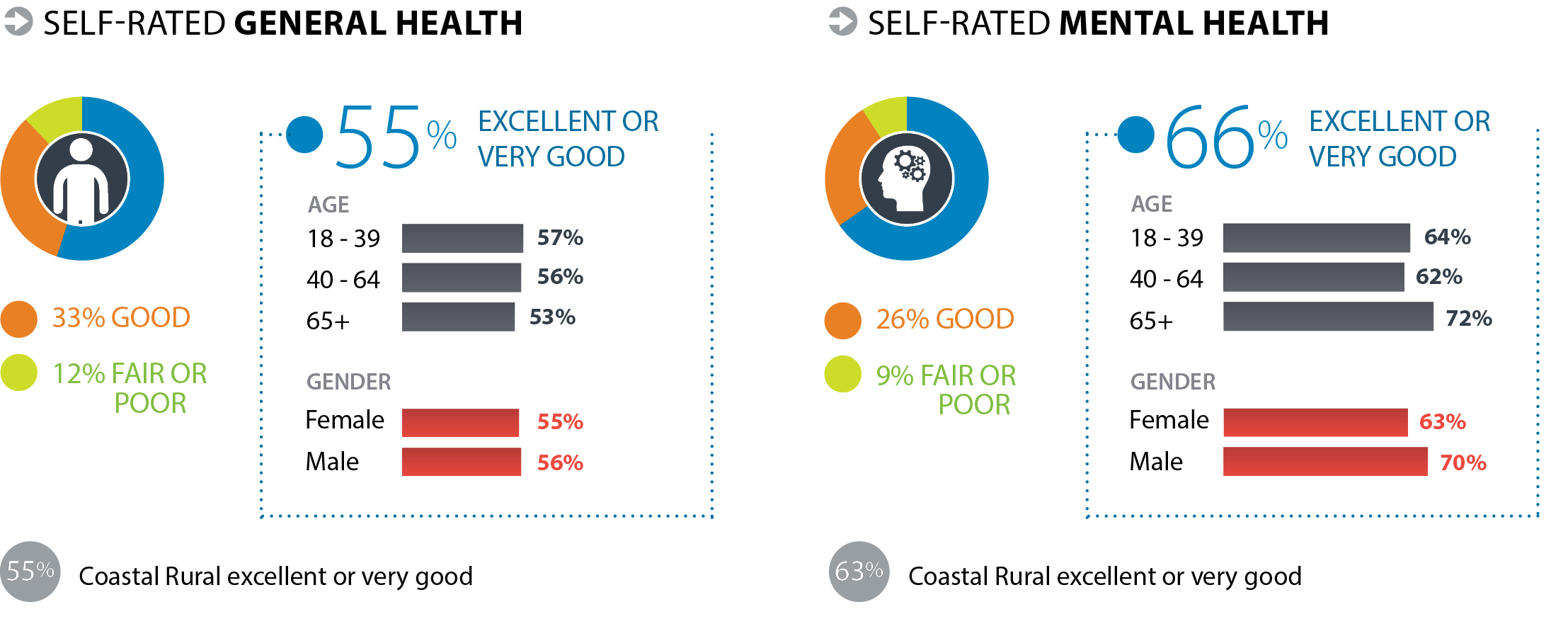
Across Coastal Rural
- University graduates were almost 3 times more likely to report excellent or very good general health and 35% more likely to report excellent or very good mental health compared to those with less than high school education.
- People with annual household income $120,000+ were 2 times more likely to report excellent or very good general health and 40% more likely to report excellent or very good mental health compared to households with annual income below $40,000.
Obesity
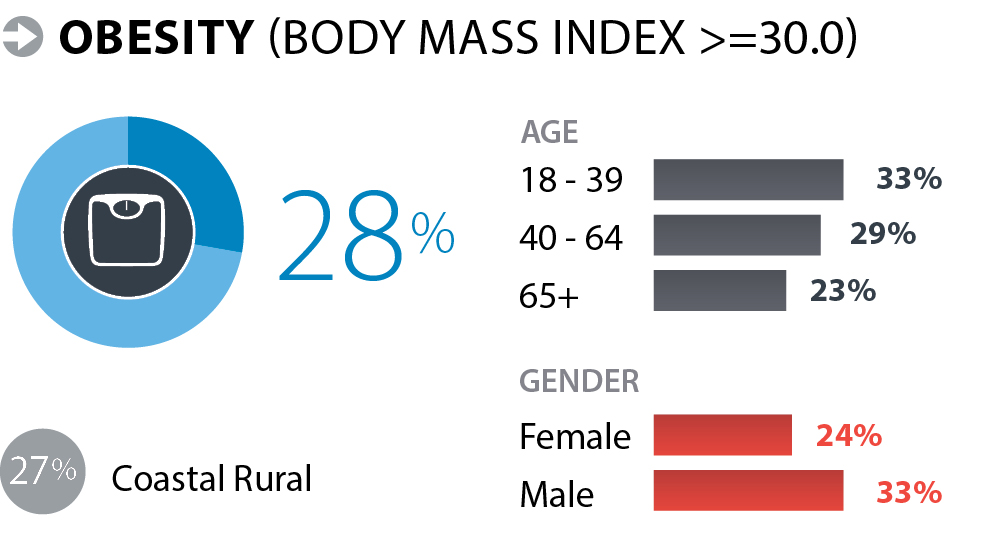
Across Coastal Rural
- University graduates were 70% less likely to be obese compared to those with less than high school education.
- Obesity was 40% lower among immigrants compared to Canadian born.
- People with annual household income $120,000+ were 40% less likely to be obese than those with annual household income less than $40,000.
Self-reported Chronic Conditions
Chronic conditions are a major burden on our health care system, individuals, families and communities. Strategies to prevent chronic conditions include the development of policies and programs, at a community level, which encourage and enable healthy behaviours in order to reduce risk factors for chronic conditions.
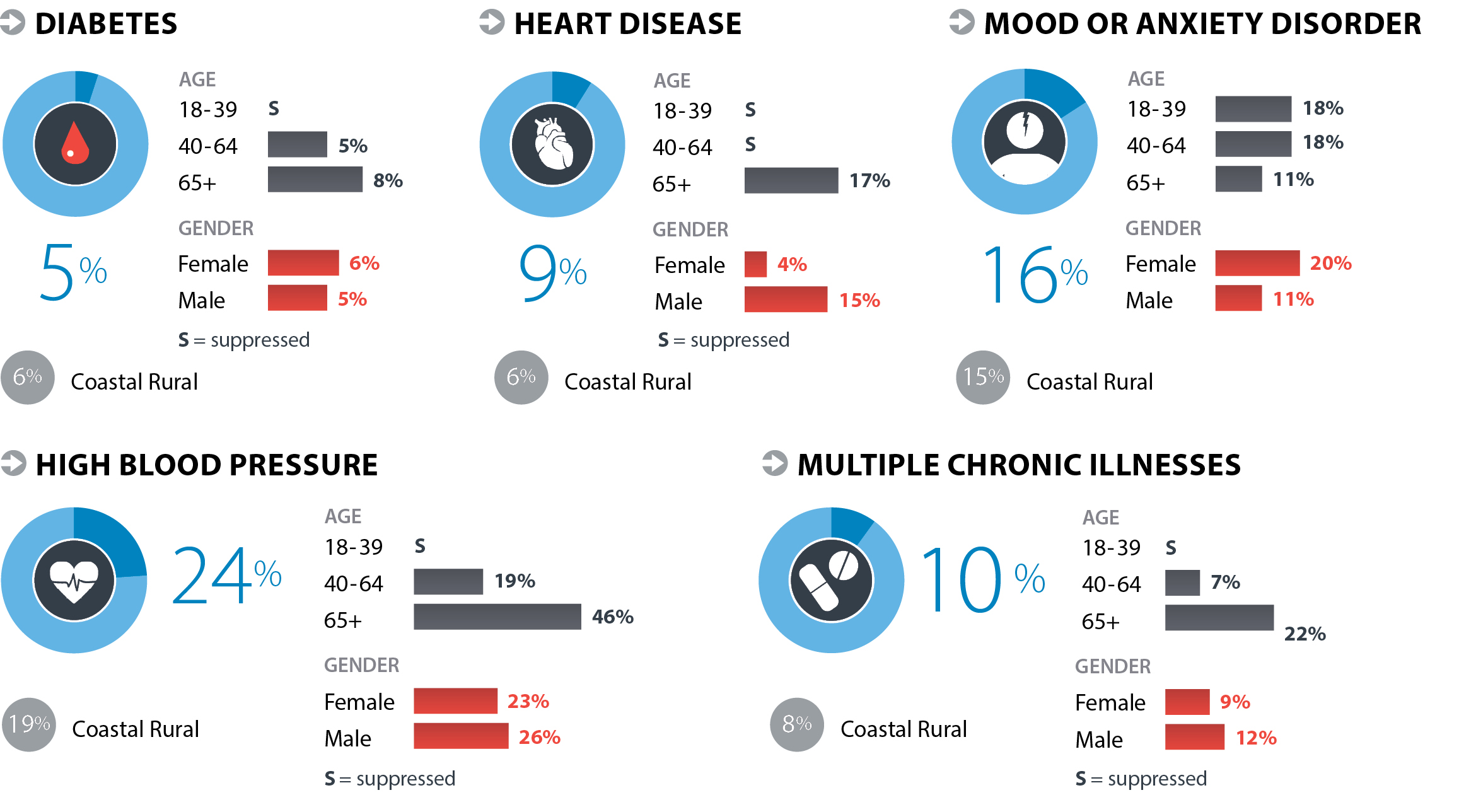
Across Coastal Rural
- Compared to university graduates, multiple chronic conditions were 5 times higher and high blood pressure was 2 times higher among those with less than high school education. Compared to Coastal Rural overall, university graduates were 60% less likely to report diabetes.
- Among people with annual household income under $40,000, high blood pressure was 2 times higher and mood and anxiety disorders were 90% higher compared to those with annual household income $120,000+.
